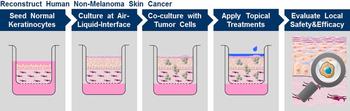
Development of human-based skin disease models
Non Melanoma Skin Cancer
Image Credit: C. Zoschke, adapting Images from Servier Medical Art (www.servier.com/Powerpoint-image-bank), 2014.
Pharmacologists of the Institute for Pharmacy, Freie Universität Berlin (head: Prof. Dr. M. Schäfer-Korting) reconstruct human skin (3D models), both normal and diseased. These complex tissues built by primary, human, differentiated cells (e.g. keratinocytes, fibroblasts) reflect a plenitude of physiological and pathological functions of human skin and thus appear suitable for the nonclinical evaluation of investigational new drugs and of toxic agents – while reducing animal studies. Skin models can be used for fundamental research, too.
Regularly, simple (2D) cell cultures constitute an inferior option, as the proliferating cells of – most often – a single type do not show the essential interaction of differentiating cells of various types forming an organ. This holds true, even for 2D cultures of human cells.
The skin holds a pole position with respect to alternatives to testing in the animal. In particular the aim to avoid safety testing of cosmetics and their ingredients in forced the development of test protocols for phototoxicity, skin corrosion, and skin irritancy in reconstructed human epidermis – the outer skin layer. Today, these test protocols are internationally (OECD) adopted. Moreover, in-vitro protocols for the preclinical prediction of cutaneous uptake and biotransformation as well as beneficial and noxious/adverse drug effects in man are established and validated.
Testing on reconstructed human organs will eliminate poor prediction of data from animal studies linked to major differences in human and animals. E.g. the murine epidermis is much thinner than human epidermis with rodent skin showing hair follicles in high density which are acting as shunt pathways for skin penetration. Thus the uptake of environmental agents and drugs is generally overestimated and mouse models of barrier deficient skin clearly deviate from human disease.
Models of non-melanoma skin cancer and atopic dermatitis are in the current focus of the scientists of Freie Universität Berlin – both are very frequent skin diseases. The skin tumor model is based on reconstructed full-thickness skin inoculated with a human tumor cell line. The varying invasiveness of the tumor can be modeled, too. Gene silencingin primary human keratinocytes is the basis for the approach to atopic dermatitis. Models of aged skin are under preparation, too, as we aim to reflect human diversity (sex, ethnics, age etc) in drug research.
Other than with the protection against the uptake of environmental agents, the skin barrier is a major problem in topical therapy of skin diseases and impairs the transdermal application of drugs posing a therapeutic problem because of rapid hepatic inactivation following oral dosing. In order to improve therapy, the group of Schäfer-Korting investigates nanoparticles for enhanced cutaneous drug delivery.
Third-party funding by the Deutsche Forschungsgemeinschaft (CRC 1112, project C02) and the Bundesministerium für Bildung und Forschung (Berlin-Brandenburger Forschungsplattform für die 3R[1]; BB3R) is gratefully acknowledged. The embedded graduate program BB3R (head: Prof. Schäfer-Korting; vice-head Prof. Kleuser, Potsdam University) allows for a broad training of junior scientists (assistant professors and PHD students) in humane research techniques.
[1] 3R: Reduction (reduction of the number of animals); Replacement (complete avoidance of an animal test); Refinement (inducing less pain and stress in the animal)